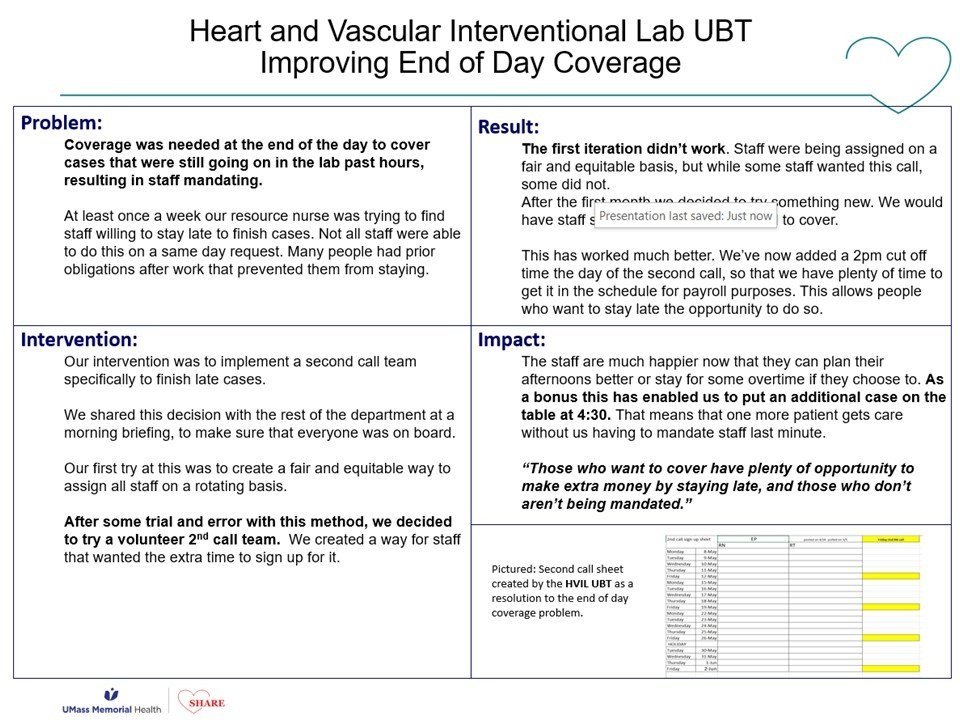
2024 IHI Conference Presentation: Unit Based Teams
Ever wonder exactly what’s getting said outside our hospital about the work you do? Continuous Improvement Coach Will Erickson had the following to say to healthcare leaders from around the country in a talk that he gave at the recent Institute of Healthcare Improvement Conference in Orlando, Florida . . .
IHI 12/10/24
Will Erickson presenting at IHI in his trademark red sweater. To see the slides from his presentation, [[[click here]]]
I’m Will Erickson, I work as an organizer and continuous improvement coach with the Labor Management Partnership Office at UMass Memorial Health in Worcester, MA. I’ve attended the Forum several times over the years but this is my first time presenting, and I’m so grateful that my friends Amar and Becka invited me to join them.
Ok, so now I’m going to tell you about how we’re improving how people feel about coming to work every day through our Unit Based Team program at UMass Memorial, in partnership with our largest union.
First, a little bit about our system: we’re a mid-size academic medical center and safety net with a bunch of community hospitals and practices in Central Mass. We’re the largest provider and largest employer in our region, so the quality of our jobs, and our care, really matters to our community. Unless I’m misjudging this audience, I’ll bet a lot of you work in places like this one.
To understand this story you also need to know about the SHARE union, which makes up the other half of our labor management partnership. It’s the largest union because it represents a lot of different job titles, like nursing assistants, medical assistants, rad techs, respiratory therapists and billers. We organized our union around the values of solidarity and voice: taking good care of each other and being able to participate in decisions about what happened to us. I say us because I come out of this union as an organizer. The lead organizer of that union, Janet Wilder, is in the audience this morning.
Coming into 2016, SHARE leaders had achieved a lot in terms of making their jobs better, but they felt that they hadn’t made a lot of progress making these jobs feel better – in a lot of ways, the work felt harder and more draining than it had. Together with UMass Memorial, we found ourselves facing a shared set of problems; a disengaged workforce that resisted changes they perceived as being done to them – no one wants to feel process improved. We suffered from unreliable processes and variable outcomes, pretty bad patient experience scores, and strained labor relations. And that’s a picture of a much younger me manning an informational picket line in front of one of our hospitals, just to prove my labor bonafides.
We looked around for alternatives, and found the Kaiser Permanente Labor Management Partnership, which is still in place today and the most important labor management partnership in place in US healthcare right now, maybe in any industry in the US. With support from Kaiser and its unions, from our own hospital’s leadership which was a couple years into a Lean journey, and drawing inspiration from a couple trips to the IHI Forum, we did something brave and formed our own labor management partnership, one that was built on those central pillars of voice and solidarity, participation and mutual respect and support.
Following the lead of our friends at Kaiser, our Unit Based Teams are built on the foundation of this labor management partnership. These are department-level process improvement teams create to help us establish a more invigorating work culture, to make labor management partnership an actual, real thing at the frontline between staff and their managers and not just for the leaders at the top. This is our effort to organize a bottom up social movement for safer, smoother, better processes.
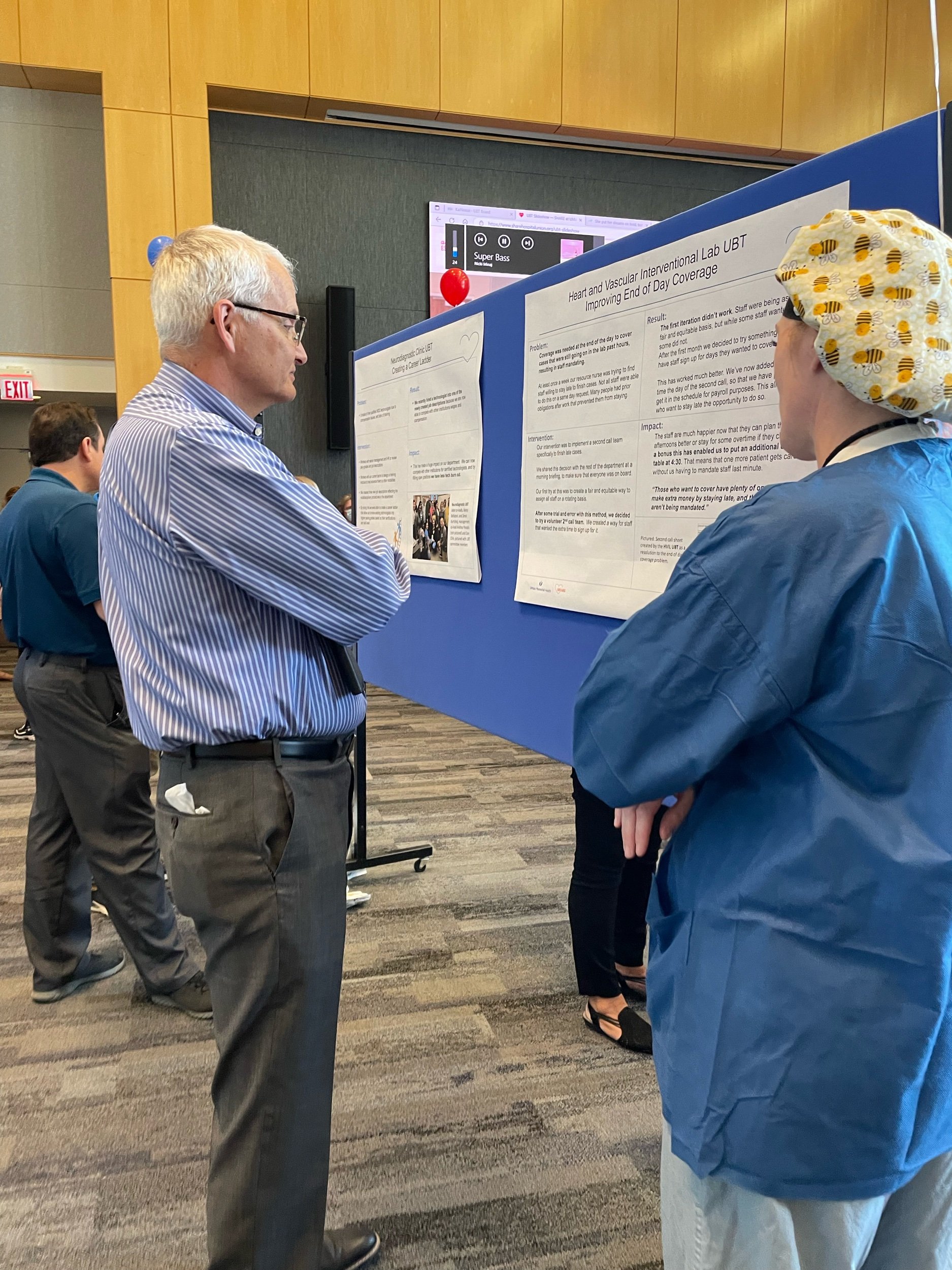
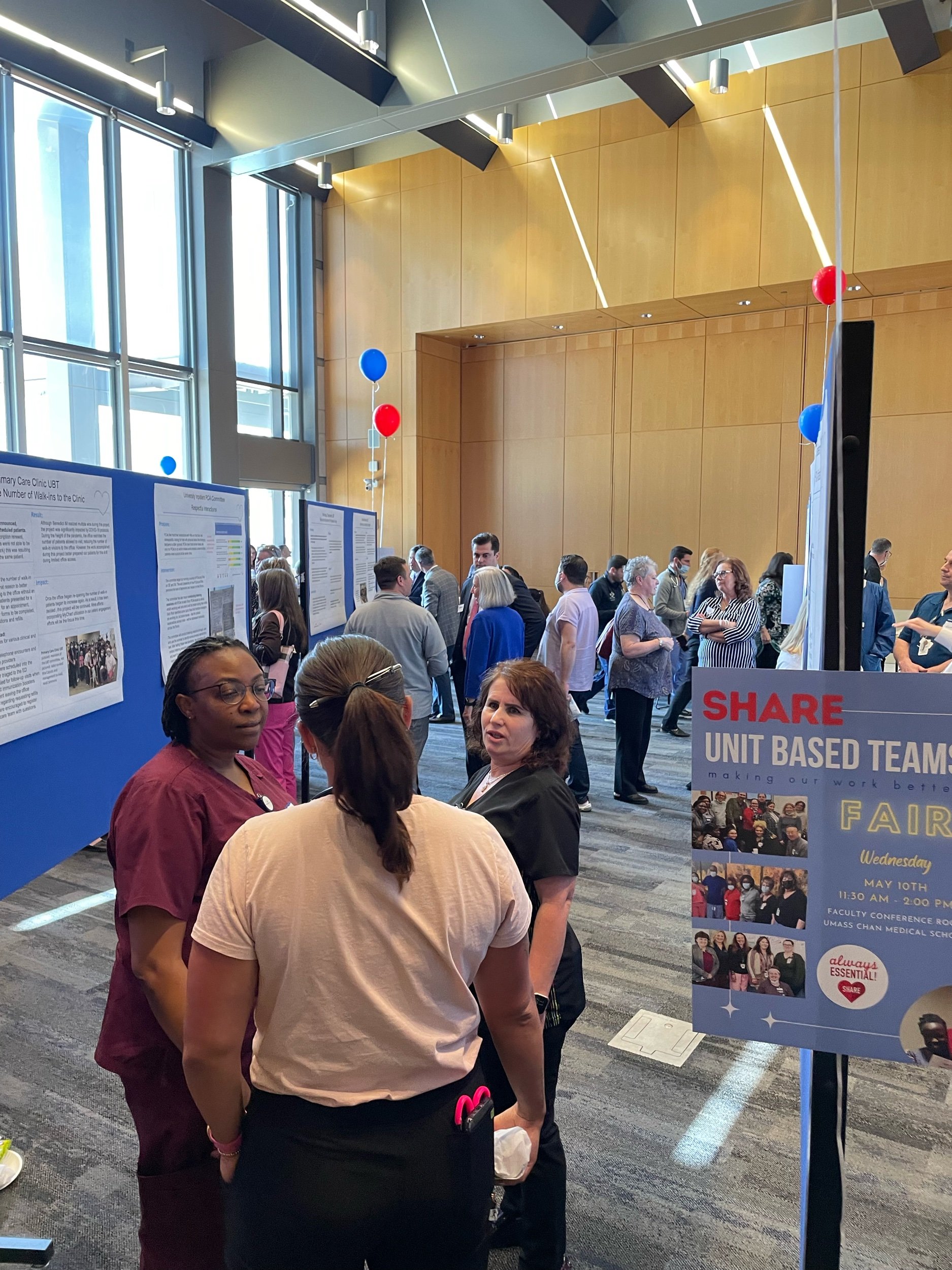
This is a picture of one of our UBT Fairs from last Spring, when we got several hundred of people together to share out posters of their favorite improvement project from the last year. One of the great things about rooting our movement for process improvement in the labor movement is that in the labor movement its still cool to belt out songs together, its one of our proudest traditions. So at these UBT Fairs we actually pass out adapted lyrics to pop songs and get several hundred people to sing together about their love for process improvement.
We now have 70 or so UBTs working on projects to reduce falls, to improve patient experience, to reduce no shows, to improve copay collection, to improve throughput. But the UBTs don’t exist for the purpose of solving those problems. The primary purpose of a UBT is to change how our caregivers feel about coming to work everyday. But the big theory of change that animates this whole program for us is that the best way to change how our people feel about their work isn’t pizza parties, or ropes courses, or trust falls, or meditation apps (we’re not against those things) but to involve our frontline people in identifying and then working to solve the process issues that are driving them the most bananas.
Each UBT has a committee of staff, providers and managers. Each is co-led by a labor co-lead and a management co-lead, and each team, in addition to having an improvement coach like me, is co-sponsored by a union leader and a management leader, usually the manager’s boss.
Most of our UBTs meet for 30 minutes every other week, and each works on 2-3 projects at a time. We encourage them to work on big issues, but to scope their project such that it can be completed in less than 100 days – I think that 100 day rule is one we brought back from one of these forums. The co-leads facilitate the meetings and prep for those meetings together beforehand. Our co-leads are really the axle around which the UBT turns, so we give them lots of training and support – we view UBTs as a vehicle for developing frontline leaders and upskilling our managers, not just for process improvement. Projects are chosen by the committee, and decisions are made by consensus. We test for consensus by asking three specific questions: has everyone been heard? Can everyone live with this decision, even if it wasn’t your first or second or third choice – will you try it? And finally, will everyone here support this decision outside this room – are we together in this? We want our improvements to stick.
So that’s the concept, but are they actually making a difference? There are several different ways to answer that question. First, our UBTs are making big, substantive impacts with their projects. One of our CT departments, for example, created a patient staging area and reduced wait times by 20% despite an increase in volume. If the management team had gone to the staff and demanded an increase in volume, the techs would have spit the bit – what stressed the techs out more than anything else was how late they were running pulling in outpatients in the afternoons – the techs wanted to see a decrease in outpatient slots. After setting up the staging area, our techs’ reported stress levels were 40% lower. Happier patients and smoother process made happy techs.
Our managers are also reporting general improvements in productivity and good feeling as a result of their UBT work – a kind of generalized halo effect. I love this quote from one of the NPs in Vascular Surgery – this department started out meeting every other week for 30 minutes, then increased that to every week for 30 minutes, and then they extended the time to a full hour because they felt like they were getting so much out of the time together.
And we’re seeing an effect in our caregiver experience survey results as well. In a recent survey departments with a UBT showed twice the improvement in engagement as our entire system, and four times the improvement in the bundle of questions that basically get at what people think of their boss. And the questions with the biggest gap between departments with UBTs and those without one were “I am involved in decisions that affect my work” and “this organization treats employees with respect”. Remember that we built our partnership on the pillars of increasing participation and improving the culture – I just love that.
Our joint improvement work is also gaining notice in the labor relations universe. Here we are with US Secretary of Labor Julie Su. She’s unfortunately only got a few more weeks in the job.
And of course the best evidence that we’re making an impact is what our caregivers are saying about how UBTs have changed them, and how they feel about coming to work. We’re not going to have time to show you this compilation, but we’ll give you the QR code at the end so that you can watch on your phone – I really hope you will.
So to wrap up, what’s different about these UBTs? First, ownership is truly shared. This is not a top down management thing, but its not just a union initiative either. That’s made it easier to leverage multiple leadership networks, especially our often unsung, informal frontline leaders, and sometimes even those grouches in the department who’ve historically been skeptical of any change. We also think we’ve created a structure that makes it easier to talk about hard things – partnership doesn’t mean that we just act nicey-nice to each other. We don’t tiptoe around the hard stuff. We lean into the process issues that are causing conflict, because we want to solve those things. And finally, with every project, every meeting, we’re teaching our people how to work together better and to solve bigger challenges. We’re doing it in a way that refreshes the manager role, positioning them as mentors and leaders, not just command and control authoritarians. And we’re challenging union reps to not just complain that management hasn’t fixed something yet, but to jump in and organize their coworkers to come up with a better way. And we’re doing it in a way that strengthens psychological safety and combats against of the real power imbalances that can make working in a team so hard.
SHARE UBTs Celebrate Reaching Top Level of Path to Performance
UMass Memorial Health and SHARE leaders recently celebrated an impressive milestone reached by two Unit-Based Teams, or UBTs. A UBT is a frontline-led, department-level improvement system that enables caregivers to work on the process problems that make it hardest for them to feel proud of the care they deliver.
This week, Dr. Eric Dickson and other hospital leaders visited the Vascular Surgery Office and Diabetes/Endocrinology departments to celebrate the teams becoming the first UBTs to reach Level 5 status on the UBT Path to Performance.
While over 75 UBTs have been launched over the last several years across the Medical Center, Medical Group, Revenue Cycle, and Marlborough Hospital, these are the first to have reached this top level of performance.
In order to progress through the Path to Performance, a team, made up of a voluntary group of employees consisting of managers, union organizers, and frontline staff, must demonstrate competence in various ways, with a focus on designing and completing improvement projects in their own department. UBT projects often tackle things such as communication or workflow. The ultimate goal of the UBT is to make their departments better places to work — more enjoyable, smoother running, and easier places to give the high-level patient care that they want to provide.
In addition to delivering to each team a traditional SHARE-UMass Partnership Office award — a balloon shaped like a number “5” — Dr. Dickson heard from caregivers about which UBT projects have meant the most to them, what they are working on now, and how having a UBT has changed how they feel about coming to work.
Congratulations Vascular Surgery Office and Diabetes/Endocrinology UBTs for leading the pack!
Click here to learn more about UBTs, and to find out more about how to launch one in your department reach out to Will.Erickson@umassmemorial.org.
SHARE Updates: PCA Pathway Program, Free English Classes, and Unit Based Teams
PCA Pathway Program Now Accepting Applications
Congratulations to the first graduating cohort of the PCA Pathway Program! They’re now on-the-job as SHARE members, caring for patients at UMass Memorial.
Do you know someone who wants to begin a career at UMass Memorial working on the nursing floors? The Patient Care Associate Program is now open to friends and family of SHARE members!
A Strong Summer for Unit Based Teams
First, the bittersweet news: after helping establish the SHARE-UMass Memorial Partnership Office over the past few years, our beloved UBT Program Coordinator, Stephanie Pepi, has accepted another job at UMass Memorial. We wish you the best in Ophthamology, Steph!
There was nothing bittersweet about the recent FMCS/LERA conference in NYC, where leaders from SHARE and UMass Memorial presented to an international audience about the importance of UBTs.
U.S. Secretary of Labor Julie Su (above, middle left) even pulled the presenters into a meeting to talk about the Labor-Management projects that SHARE members are pioneering on the front lines.
SHARE members Celebrate success — and Share what they’ve Learned — at the 2024 UBT Fairs
The most exciting news for Unit Based Teams this Summer is the fantastic success of the UBT Fairs on both the Memorial and University Campuses, where SHARE members showed off their projects to over 1000 attendees. If you missed it, be sure to check out the most recent UBT Newsletter!
Free English Classes for UMass Memorial Caregivers
UBT Fair 2024 Newsletter
2024 UBT Fair
SHARE-UMass Memorial Unit Based Teams Newsletter
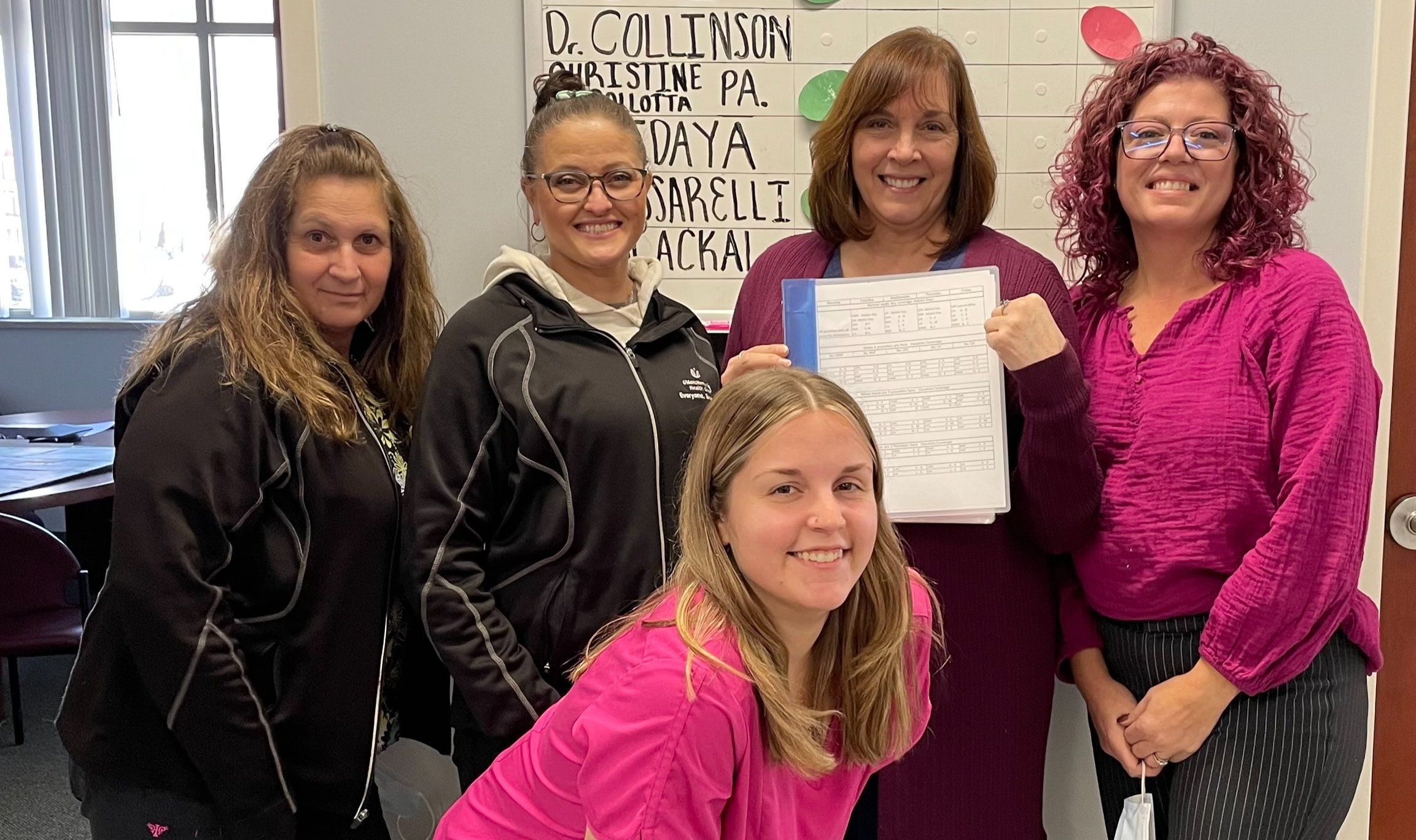
Vascular Surgery Office UBT Reaches Level 4!
The Vascular Surgery Office UBT is among the first in the System to reach LEVEL 4 (High-Performing UBT) on their Path to Performance! That means they’ve hit some serious milestones, and established themselves as a strong team. They’ve presented their work recently to the SHARE-UMass Memorial Leadership Council (LMPC), and it’s clear that their teamwork is turning into some real fun.
Frontline SHARE members in this UBT have developed projects that have yielded measurable and sustainable improvement, and they communicate and celebrate regularly about the work and successes with the whole department.
This Unit Based Team works in the Medical School on University Campus. It is co-led by Beatrice Edmonds and Devon Germak, and is co-sponsored by Jana Hollingsworth and Stephanie Costello. The UBT Committee members include Mary Borrelli, Jeanne Magliaro, Norma Mills, Lindsey Carr and Hannah Akoto-Kesse.
Please congratulate them on their big accomplishment if you see them around!
SHARE Partnership Special: New Videos, UBTs in the National Spotlight, and More!
SHARE has designed, negotiated for, and cultivated the Unit Based Team program as a powerful way for members to be directly involved in the design of our own work. This special newsletter highlights exciting developments since the recent success of the UBT Fair.
SHARE Members on Youtube
With the help of our parent union, AFSCME, we’ve developed three short videos featuring SHARE members who describe what UBTs are, the successes they’ve had, and how the teams make a difference in their work.
All three UBT videos are now prominently featured on the SHARE homepage. Check them out! See anybody you know?
UBTs in the National Spotlight
The US Department of Labor has highlighted the Unit Based Teams in a few of their recent publications and presentations. Read more on the SHARE blog . . .
Congratulations to SHARE member Wanda Dyer, who was quoted in a recent nationwide DOL bulletin, where Wanda describes, “The Labor-Management Partnership between the hospital and the SHARE union allowed us to be involved in a Unit Based Team (UBT) where I was comfortable talking about the challenges in the workflow.
New UBT Coaches
The joint labor-management SHARE-UMass Memorial Partnership Office is growing! UBT experts Will Erickson and Stephanie Pepi have recently been joined by two new UBT Coaches: Jackie Zhou and Joan Perreault. Both have previously worked at UMass Memorial, already demonstrate exceptional skills, and we think they’re fantastic. They’re eager to help support SHARE members to make the current teams stronger and expand UBTs so that even more SHARE members can participate. Welcome Jackie and Joan! We’re excited you’re here!
Welcome to new UBT Coaches Jackie Zhou and Joan Perreault!
First Ever SHARE UBT Fair a Fantastic Success!
The first ever SHARE UBT Fair is one for the books: a brilliant event showcasing projects completed by twenty-three different teams.
Over 600 caregivers in our hospital community came to check out SHARE members’ successes and learn ways to make work better in their own departments.
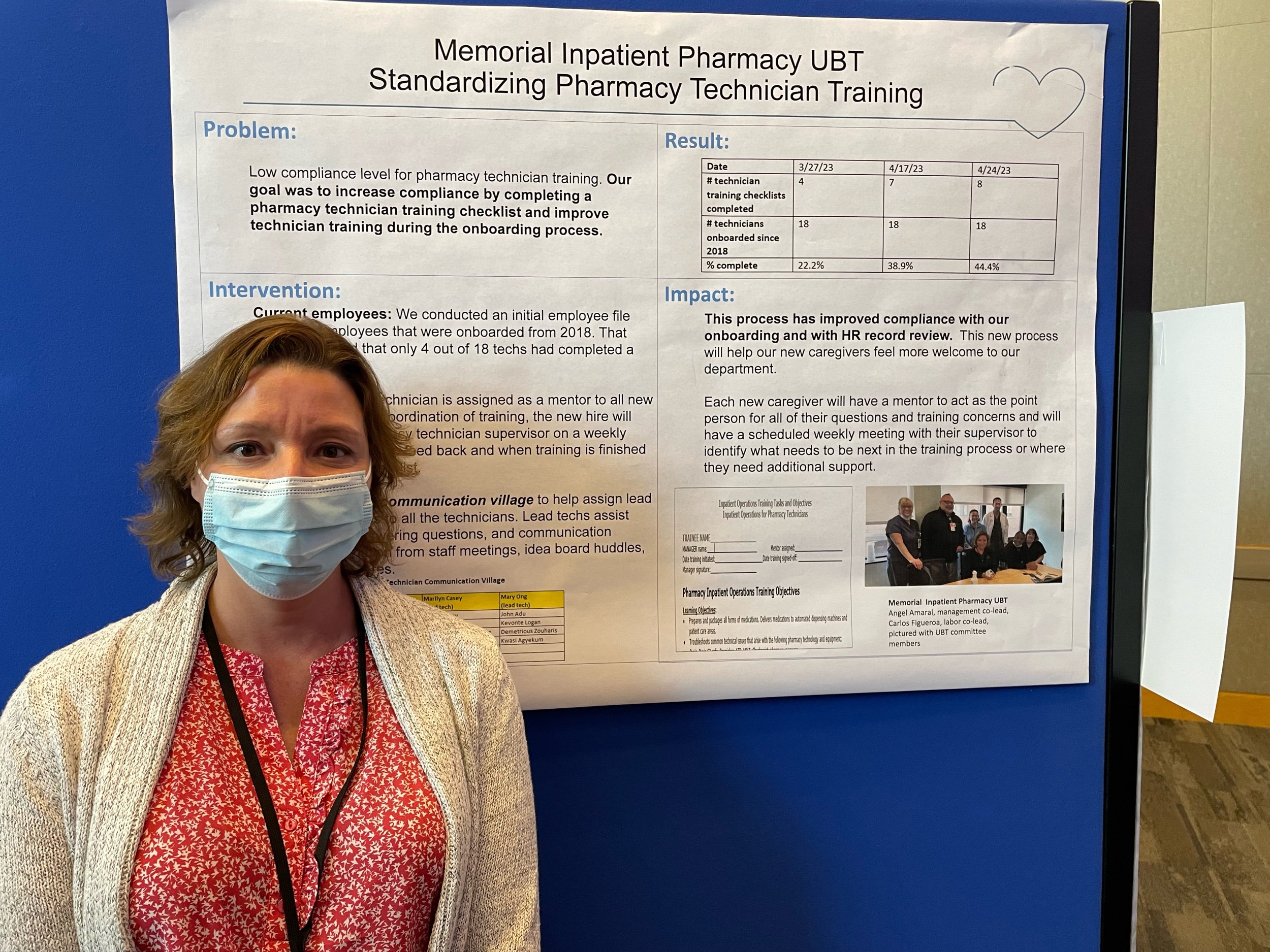
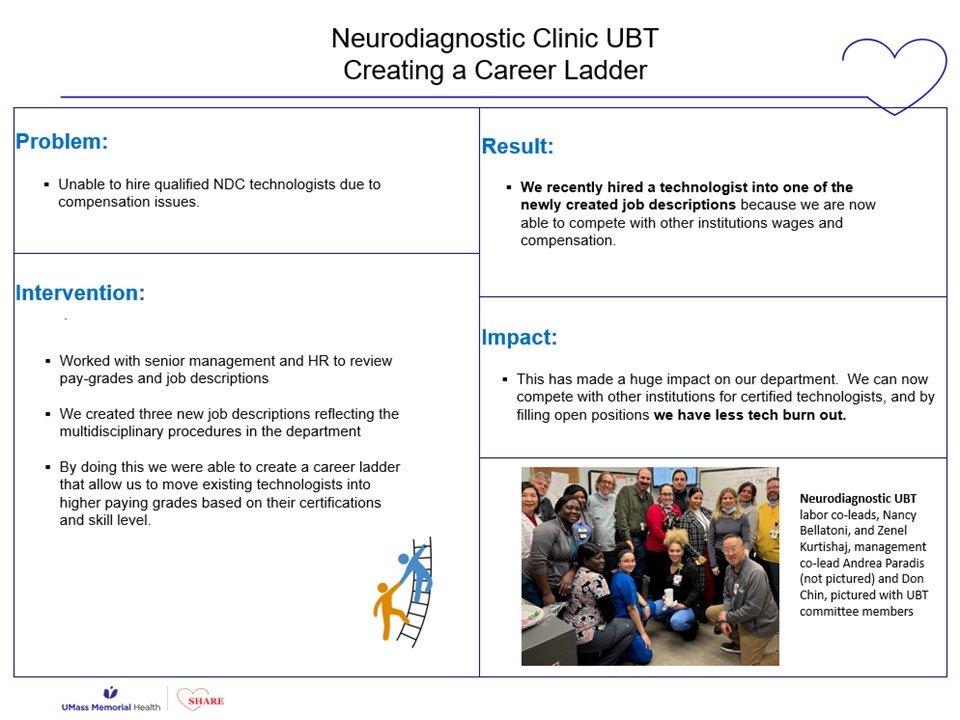
SHARE members discovered models for improving systems where they work. For example, the Neurodiagnostic Clinic developed a career ladder for staff there to grow and advance in their career, right in their own department. Seen above are NDC Co-Leads Don Chin and Zenel Kurtishaj.
Projects are designed to make the work better in a department . . . but often the results can be felt downstream, making things better for other caregivers as well.
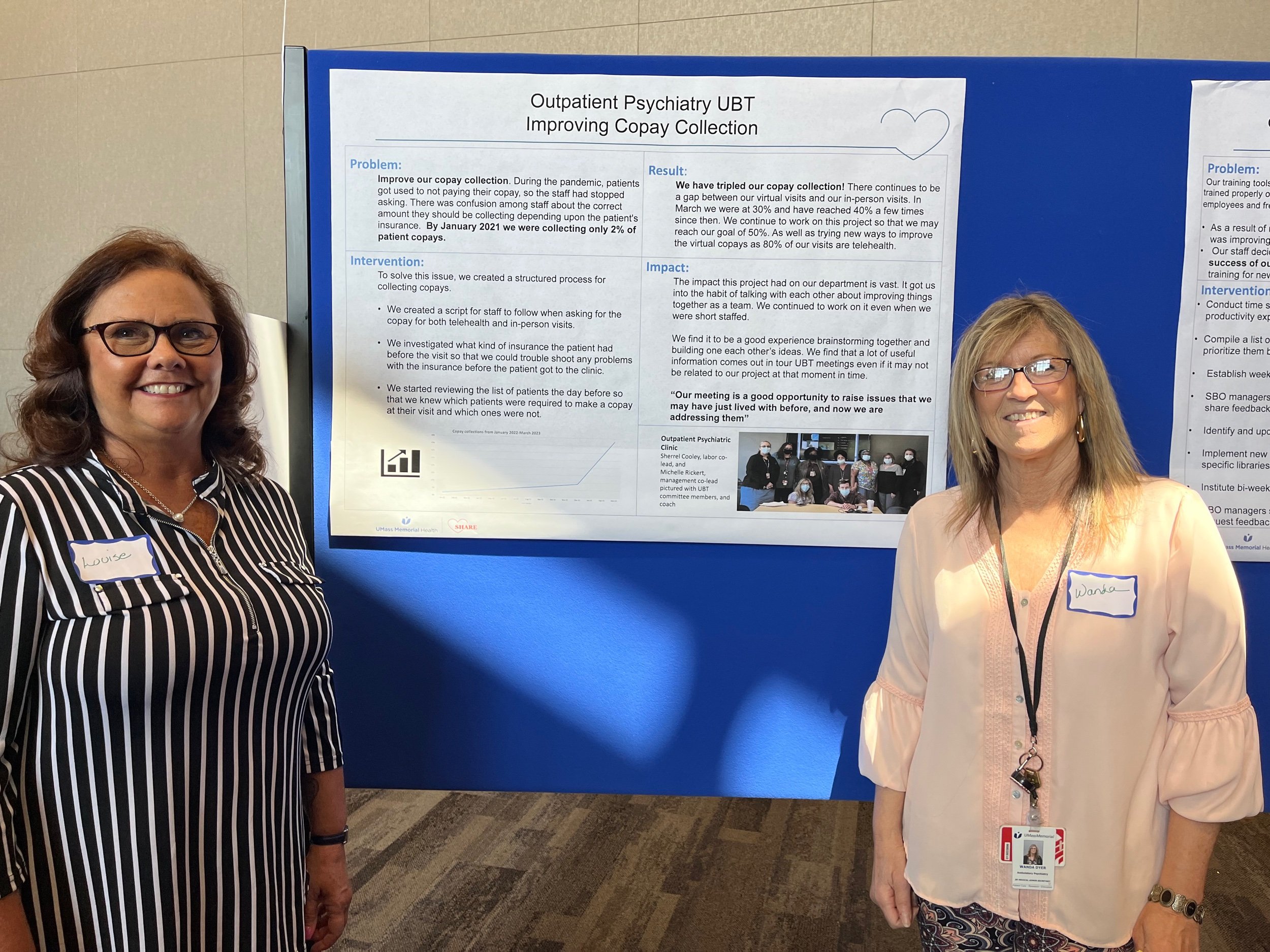
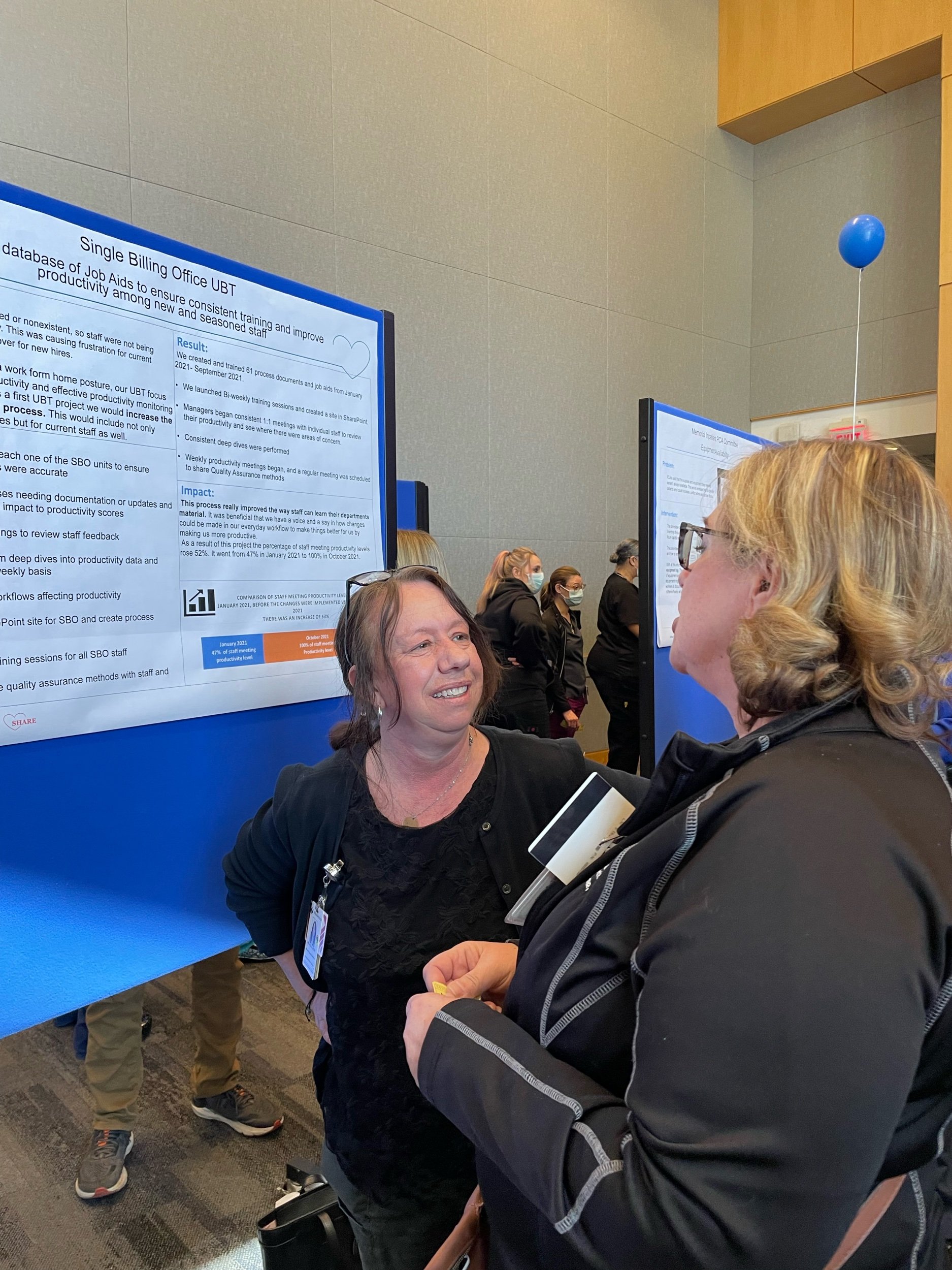
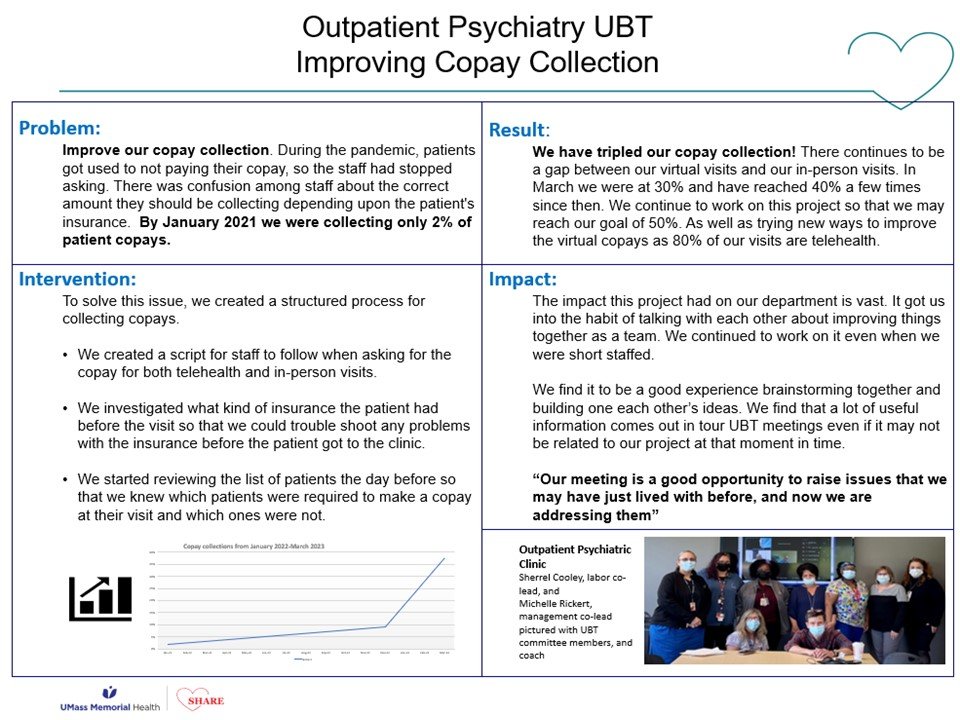
Michelle Locke (above right), management co-lead of the UBT in the Single Billing Office, appreciated the project co-lead by SHARE member Wanda Dyer of the Outpatient Psychiatry Lean Team (above left). Maximizing co-pay collections at the time of service reduces the amount of follow-up work required down the line.
Representatives from the United States Department of Labor made the trip to see just what was going on here. Labor-Management Partnership Coordinators Darnice Marsh (above, far left) and Andrew Hasty (above, far right) are among those in federal leadership working to understand ways that Labor-Management partnerships like our own can serve as a model for broader improvements.
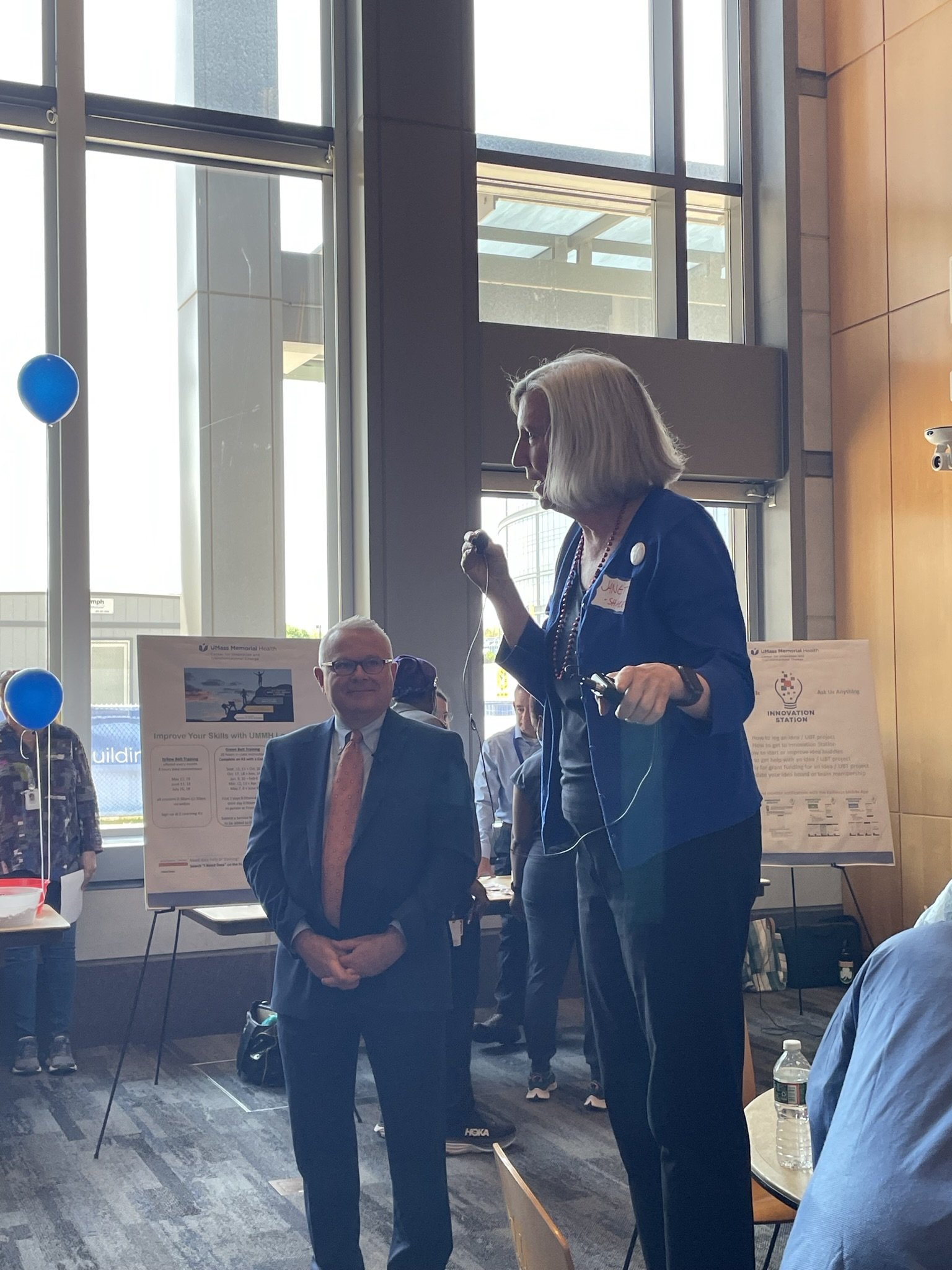
SHARE organizer Janet Wilder (standing on chair) and UMass Memorial Medical Center President Michael Gustafson (left) applauded the work of the Teams. Janet said that, during our union’s twenty-five year history, changing how it feels to come to work every day has been one of the toughest nuts for SHARE to crack . . . but UBTs have begun to do just that, and that we’re going to keep working to keep things getting better.
Incidentally, if you’ve ever been to a SHARE event before, you know that there had to be singing. This time, “The Locomotion” and “Hotel California” became victims to SHARE’s parody lyrics team.
UMass Memorial CEO Eric Dickson offered a video message of support for Unit Based Teams, citing his own belief that people closest to the work have the best ideas about how to make things better.
Dr. Dickson says that over the past ten years, the hospital system has implemented over 100 thousand frontline staff ideas, and affirms that “without reservation, the huddles that I’ve attended that are a part of the SHARE UBTs are the best in the healthcare system.”
Watch Dr. Dickson’s brief message by clicking the image above.
Everyone who came to the event was a winner, of course, but only one person could go home with the Signature SHARE Chocolate Raffle Basket. Congratulations to Nuclear Medicine Technologist (and SHARE member) Maria Nolan!
Learn more about UBTs at
www.sharehospitalunion.org/unit-based-teams
or contact
The SHARE-UMass Memorial Partnership Office
More scenes of partnership can be found online in the growing Partnership Gallery . . .
Barre Clinic UBT Solving the Case of the Missing Lab Orders
The Barre Clinic is at it again, having completed a second project thanks to their department’s Unit Based Team. Patients had been arriving to their lab appointments too often with no active orders to complete the labs. After brainstorming what was causing the problem and how they might best solve it, the team came up with an intervention that everyone could agree to try. Ambulatory Service Reps began checking for orders when scheduling lab appointments, and lab staff started entering orders in real-time for any outside orders that were faxed to the clinic, rather than waiting until the patient arrived.
By making these changes to their daily workflow, the staff have seen a decrease in the number of patients arriving without orders. It used to be common for patients to arrive at the lab without orders, now it is a rare occurrence.
“It cut out a lot of extra work,” says UBT Co-Lead Amy Moisan. Staff are no longer chasing down providers to get orders or ask what labs need to be drawn, and patients no longer wait in the clinic while they look for orders and enter them, saving both patients and staff precious time.
UBT Spotlight: Hahnemann Internal Medicine & The Book of Knowledge
CMG Hahnemann Internal Medicine UBT creates a Book of Knowledge for their clinic so that staff can easily access information
The Unit Based Team in Hahnemann Internal Medicine has created a way to make everyday information — as well as not so frequently asked questions — easily accessible to their staff.
The staff in the clinic found that they were wasting time looking for answers to commonly needed information. They were spending time looking through saved documents and emails to find answers to everyday questions such as accepted insurances, phone numbers, CPT codes just to name a few.
So, they gathered up the information that they had saved in various places to create a binder, or “The Book of Knowledge.” Now, each time they receive new information of value, they add it to the binder so that it is easily accessible.
It’s an uncomplicated idea with a fun, grandiose name. But coordinating this information has saved the staff a lot of time, giving them instant access to needed forms, cutting down on wait times to find information, and having everyone on the same page when giving information to their patients. “Now that we have pertinent information at our fingertips,” says management co-lead Katherine Auger, “the patients can receive correct information from all staff in a timely manner.”
Reach Department Goals by Aligning your UBT Project!
A Unit Based Team (or UBT) is a group of frontline employees, managers, and physicians from the same department who come together to work on meaningful projects to improve caregiver satisfaction and patient care, while improving the way they feel about coming to work every day. This project does just that!
Rheumatology Department UBT Improves Communication about Wait-Times
Department metric: improve patient satisfaction.
As a first project to work on, the UBT in the Rheumatology Department on the Memorial campus chose to communicate better with their patients about wait times once they were roomed.
An example of the timer outside a patient room in the Rheumatology Clinic
How did they do it?
The UBT worked to to re-educate the staff on timer protocols; a schedule was put into place to check on the timer batteries, and a standard location was established to ensure the timers are in the same location outside of every exam room, so they are not overlooked. The staff would then check-in with the patients according to the timer to communicate the wait time and offer some water.
The Results?
The results are positive! Caregivers now update patients more frequently about their wait times. And that’s provided additional opportunities for communication between patients and caregivers.
These check-ins have increased patient satisfaction and improved Press Ganey patient comments regarding wait times. Caregiver satisfaction improved, too!
This worked so well for their clinic, the members of the UBT were asked to present it at the All-Managers Meeting!
Way to go, Rheumatology!
Psychiatry Lean Team UBT Kicks Off New Improvements
Another Unit Based Team is on their way to making positive change at UMMH!
UBT committee members at the department orientation at
100 Century Drive . . . attending both in-person and virtually
The Psychiatry Lean Team at 100 Century Drive recently came together to form a UBT. They started to meet and work on several projects a few months ago. We’re looking forward to seeing how these projects develop.
The UBT is already experiencing a change in the way the department communicates. “It has been helpful for the team; everyone wants to be heard and this allows the perfect venue for this to happen,” said Management Co-Lead Michelle Rickert
Their UBT committee includes:
SHARE Co-Leads, Sherrell Cooley and Wanda Dyer
Management Co-Lead, Michelle Rickert
Management Co-Sponsor, Derrick Tallman
SHARE Co-Sponsor, Carol Hehir
SHARE Updates: Poster Unveiling Event TODAY, New Negotiations Website, Spotlight on the Memorial Inpatient Pharmacy
Don’t Forget: 2022 Signature Poster Unveiling Event TODAY!
Over 2,400 SHARE members signed-on to our statement in support of a strong contract before it was time to send to the printer. Today we the reveal the poster in all of its glory. If you’re on the University campus, we encourage you to come to the big event. Come find your own signature on the poster, bring a copy back for your department, and enjoy a free sandwich. (More details on the flyer below.)
You can also pick up a poster at signature events including Memorial campus next Wednesday [[details]]. More sites, including for employees with work-from-home arrangements, will be announced soon.
New Contract Negotiations Website
The best way to find out about what’s happening in contract negotiations is to come to information meetings and talk with SHARE Reps and Organizers firsthand. So you can always have useful information at your fingertips, we’ve also dedicated a new section of the SHARE website to round up contract negotiation resources. On the new site you can find:
Links to negotiations updates & contract event announcements
Answers to Frequently Asked Questions about negotiations
“Always Essential” graphics (with directions about how to add them to your email signature or virtual meeting background)
And lots more ways that you can support a strong contract!
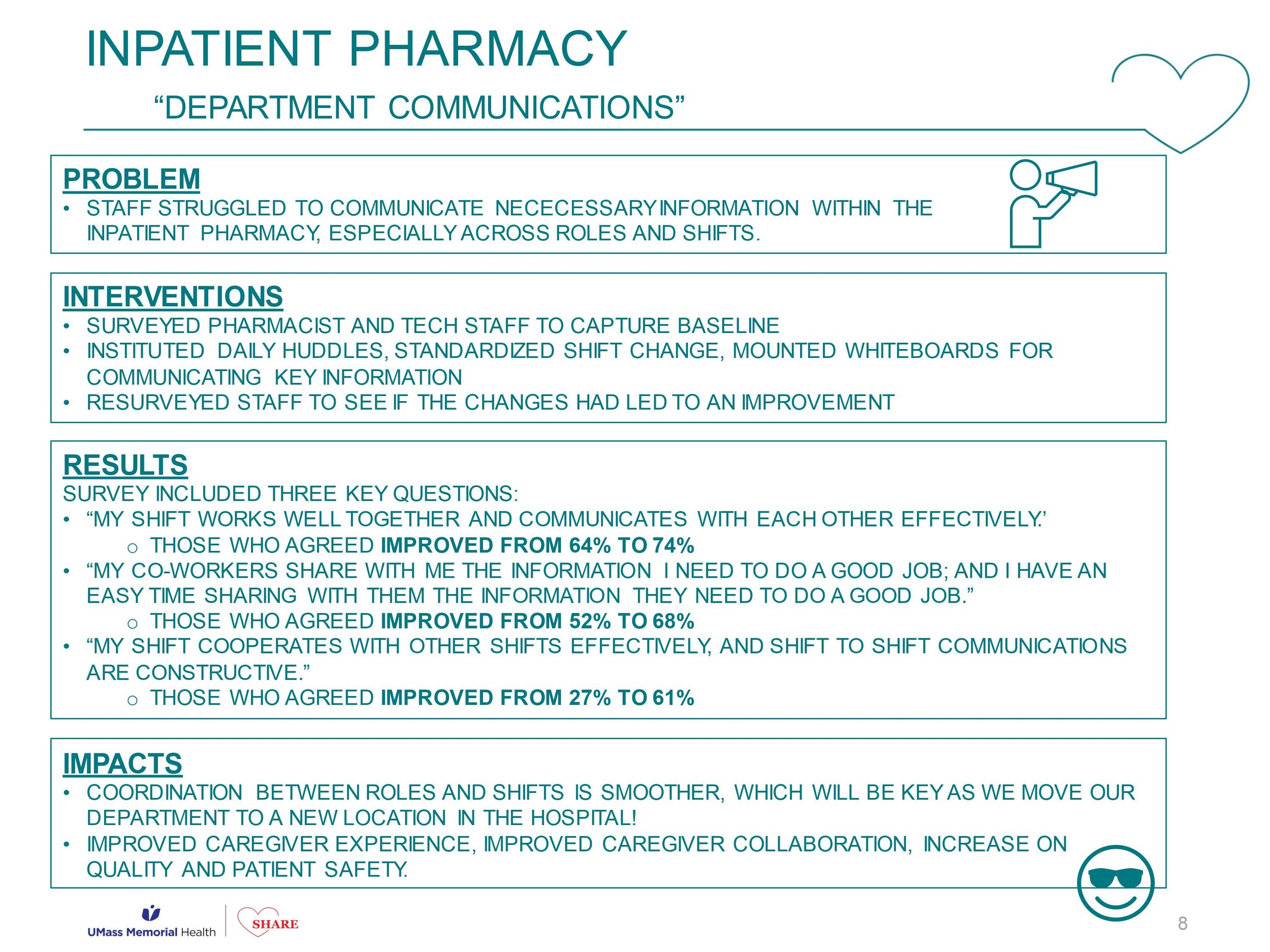
UBT Spotlight: Memorial Inpatient Pharmacy
Congratulations to the Unit Based Team in the Memorial Inpatient Pharmacy! SHARE members and other staff there are now experiencing smoother transitions among roles and shifts, thanks to a project designed to measure and improve communication. Learn more about how they did it in this UBT Spotlight post.
SHARE Updates: Negotiations, Signing On, Wearing Red, and More
YOU Can Help SHARE Bring Home a Strong Contract!
Through countless conversations and survey responses, you’ve told SHARE what matters to you. Our negotiating team is making the case to the hospital that it needs to invest more in SHARE members. We need meaningful raises. Here are some ways to support SHARE now:
Sign-on to the 2022 SHARE Poster for a Strong Contract. If you already signed — thank you! If you haven’t already, we urge you to do that asap! Just talk to the SHARE Rep in your area, or call or email the SHARE office.
Wear red on Thursdays to show solidarity with the negotiating team as they meet with management.
Every day is a good day to wear your SHARE “Always Essential” button!
Stay informed! Read on below to learn what’s happening now. For a look back at recent updates, check out posts marked #Negotiations
SHARE members in Urology are wearing their red! Pictured here are SHARE Union Rep Miranda Leger, LPN; SHARE Union Rep Yvonne Ashworth-Thayer, LPN; and SHARE member Alexandra Towouh, LPN
Negotiations Update
Our negotiation sessions are still all about the money. After presenting initial proposals, both teams have made adjustments to their positions in response to the interests we’ve heard from each other. In case you’ve missed it, SHARE’s proposal is designed to:
Take inflation and the rise in cost-of-living expenses into account.
Make sure SHARE members make progress every year as their experience grows.
Catch up to what other employers are paying so that UMass Memorial can hire and fill positions, so SHARE members aren’t so short-staffed.
Deal with the fact that the rising minimum wage in Massachusetts, added to the national staffing shortage, makes it especially hard to retain staff.
Recognize SHARE members’ hard work during COVID and now – SHARE members are Always Essential!
Negotiations Update: Side tables
While the main Negotiations is all about the money, two side tables are focused on other good things for SHARE members. The “Leaves & Absenteeism” side table continues to work to streamline the Leave of Absence programs. SHARE wants to make it easier for you to understand what programs are useful to you, while at the same time retaining the job protections currently available.
The “Career Advancement” side table is exploring ways to make it easier for you to get the education you want and to grow in careers at UMass Memorial. SHARE and management members had an exciting meeting with representatives from the Ben Hudnall Memorial Trust (BHMT) at Kaiser Permanente, a nationwide healthcare provider network based on the West Coast engaged in Labor Management Partnership. The BHMT has developed over the years to help over 110,000 union members have access to training and academic degree programs with zero out-of-pocket costs. Their system provides a useful model for what our hospital and union could do right here.
SHARE Testifies for Bed Expansion
SHARE testified in support of adding beds at the Massachusetts Department of Public Health virtual hearing about UMass Memorial’s application to add 91 new inpatient beds: 72 at the “NIB” (New Inpatient Building, the old Beaumont nursing home building next to University Campus), and 19 at Memorial.
In her testimony, SHARE Organizer Janet Wilder described how difficult it is for SHARE staff to provide care in these circumstances: feeling bad for making patients wait, always juggling, always running – it’s exhausting! Read the full post here . . .
Updates from the SHARE-UMass Memorial Partnership Office
SHARE’s Unit Based Teams continue to expand and make important strides toward improving how it feels to come to work in our hospital. And the SHARE-UMass Memorial Partnership Office continues to develop new ways to support those teams. We’re excited to hear these new updates from them . . .
PCA Committee Off to a Strong Start
Congratulations on launching your team!
Already got a UBT? Check this out . . .
Unit Based Teams Peer-Learning Event
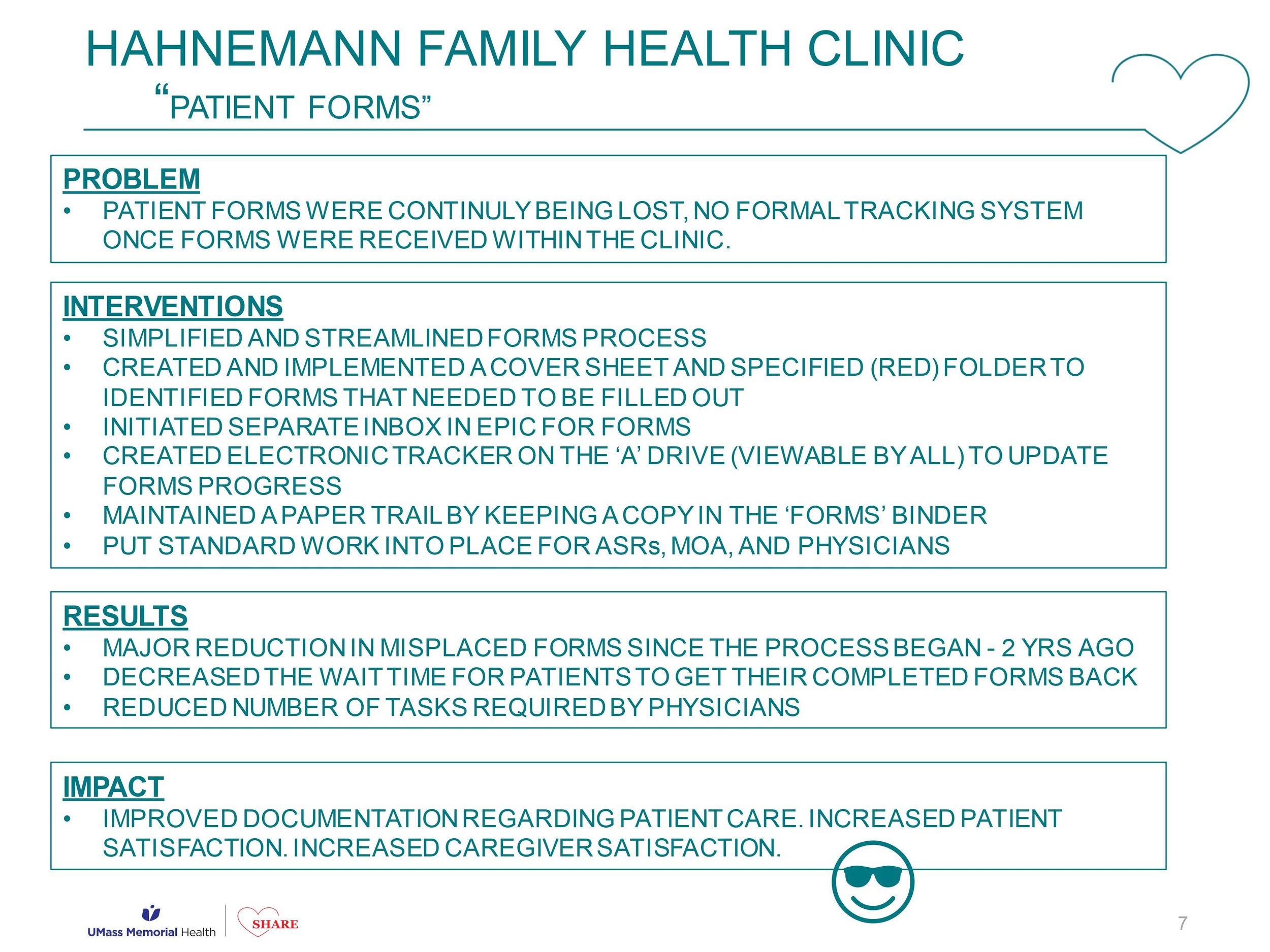
Heidi Brazeau, SHARE UBT Co-Lead, describes to the virtual crowd how her department improved tracking the many different forms that patients bring for them to process at the Hahnemann Family Health Clinic
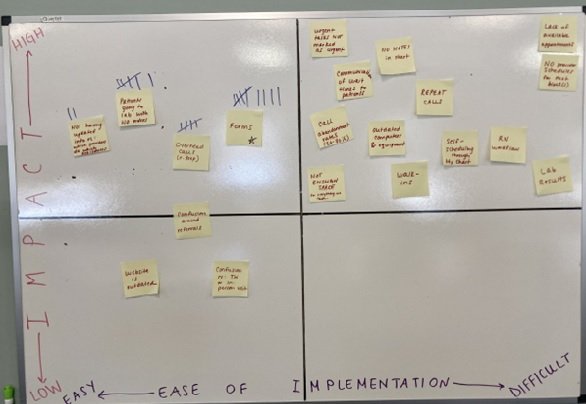
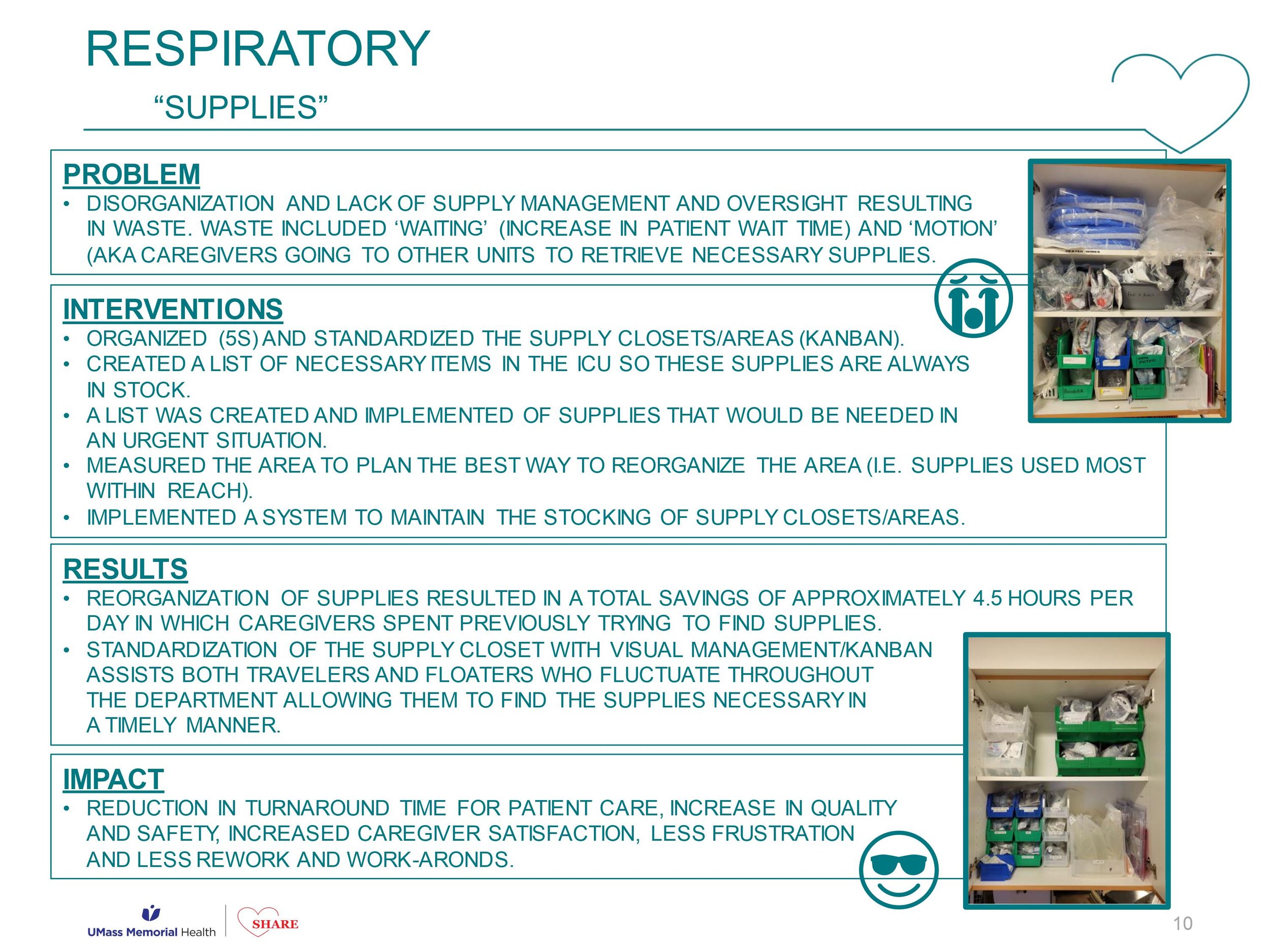
Earlier this month, twenty-plus UBT Co-Leads from SHARE and management met online to compare notes about what makes for a successful project. Four teams — Hahnemann Family Health Clinic, Inpatient Pharmacy, Rheumatology, and Respiratory — each presented about a project their team had undertaken. They described how the project made things easier for staff in their department, what it’s done to improve patient care, and why the department is better able to take pride in their work as a result. In each case, these particular teams chose to develop some kind of system for themselves that created standard work that suited the needs of their department.
Congratulations to each team for these successes! Check out the slides below for details about each. . . .
UBT Shout-Outs: Barre
A new Unit Based Team kicked off their first meeting in Barre on April 8th. They have begun meeting every other Friday. They spent their first two meetings brainstorming ideas and have decided to work on creating a standard work process for forms. This will include disability, workers comp, FMLA, etc., with the aim to reduce the number of patient inquiries after dropping the forms off as staff can advise them on timelines, in addition to keeping the paperwork better organized. You’re off to a great start, Barre!
What's New with Unit Based Teams?
SHARE is excited about a number of recent developments involving Unit Based Teams, or UBTs. Our UBTs, and our union’s partnership with UMass Memorial in improvement work, are designed to change SHARE members’ everyday experience of being at work.
Most UBTs had to pause their improvement work during the omicron surge, but are now getting back into a regular cadence of meeting and working on projects selected by members on the front line. Here are some highlights:
If you see her in the halls, be sure to say hi to Crystal . . . you may remember her as a SHARE member and an employee of the Radiology Department
The Partnership Office is growing! We welcome back former SHARE member Crystal Swenson as she re-joins our hospital as a new UBT coach.
UBTs are now tracking their work using UBT Boards on Innovation Station
A new UBT Toolkit is up on the hub
SHARE leaders are helping UBTs find and fund equity work
New UBTs are currently launching in
Pre Surgical Evaluation (Memorial)
Endoscopy Suite (University)
Endoscopy Scheduling (Hahnemann)
Barre
Heart Station
Rheumatology
You can learn more on the UBT page of the SHARE website and in blog posts marked #UBTs.
UBT Spotlight: Pediatric Clinic
Pedi Clinic Unit Based Team (left-right): Pat Labbe, Anne Taylor, Maureen Guzzi (UBT Management Co-Lead), Jen McRell (UBT SHARE Co-Lead), Marnie Doyle (joining the team on the phone), Cassie Steele, Marie Manna (UBT Coach), and Joanne Hunt
The Pediatric Clinic Unit Based Team (UBT) is a group of enthusiastic, thoughtful staff with a good sense of humor. In the discussions we’ve had on various topics, it’s clear that they care about their patients and their families . . . which, of course, leads to thinking about patient satisfaction as a high priority. The UBT has done valuable work over these past 3-4 years in taking on projects that improve work processes that benefit the patients, the staff, and the hospital. Some of these have involved streamlining processes like ordering a urine sample, paperwork needed, and communication within teams. All of this work helps to save wasted time, increase efficiency, and leads to more satisfied patients and staff. One particular project that helps the hospital was improving the wrap-up process in order to collect hundreds of thousands of dollars more in payments in a timely fashion.
I have very much enjoyed coaching this UBT, and - since they are so enthusiastic (read, “passionately talk a lot”) — I’ve had to use my coach’s time-out signal more frequently with them than with some other UBTs. While all members are enthusiastic, they each understand and appreciate the need to listen closely to one another which has built strong, respectful relationships. Their “enthusiasm” is a visible indicator of their commitment to their work, the patients, and each other.
—Marie Manna, UBT Coach
Jen McRell and Maureen Guzzi: Pedi Clinic UBT Co-Leads
Interview by Anna Weick, 2/23/21
J: In the Beginning, we didn’t know what to make of the Unit Based Team. But within a few weeks, people started feeling comfortable enough to come to us with ideas and things we could work on in the meetings. It did take a few weeks to get it up and running and get people on board with it.
M: So, Jen and I have been together on this since the get-go. The UBT project was presented to the managers and we sent it out for volunteers. We tried to gauge interest and see who wanted to join. I had a core number -- not a huge number -- of people interested. Jen was one of the people who came to me and said she was interested, and she became my co-chair. The people who are currently on it have pretty much the people who have been on it since the get-go. We have had some people leave, and we’ve brought a few new people in. But for the most part, it has been led by the same people and same team who were interested in the beginning. While we might get more interest now, we encourage people to speak if they want to join, or to give us suggestions. Like Jen said, we originally met about almost 3 years ago. We met, we defined, with our coach Marie, who comes to all our meetings -- who guided us to where we wanted to go.
The staff went back out to talk to the other staff. Within a couple of weeks we had about 20 ideas when we first started this. We all met together and put the ideas in order of priority, and then we started to tackle them. We recorded it, took minutes, posted it on our UBT board in our lunch room area. We went through about 12 of those 20 things in the first year, putting them in order, starting one and seeing it through. Some of the stuff over the course of the year, it self-corrected. So the next year we talked about the next big three projects we wanted to take on. We tackled those three projects -- we probably weren’t as ambitious as when we originally started because we had a lot of small projects to go through.
This last year we just met again, we looked again at the True North metrics for the organization, and we tailored what we want to accomplish around those.
J: And then Covid happened . . . everyone got deployed for a while.
M: Coming back we learned that -- reuniting back together was really challenging for us, so we had to spend some of our time on rebuilding the team. It was hard during deployment.
J: And then going into new roles, with coming back -- now there are telehealth visits, and things not in person. It’s a whole new work environment that a lot of us weren’t used to. So, getting together and coming up with rules for that too.
M: Normally they knew what they did every day. They did the same things pretty much every day. While you say you want to implement something new, we found the challenge is, well, you can’t just say ‘go do the telehealth,’ because no one knew how to do a telehealth. And then, when we thought we knew how to do the telehealth, the people doing the telehealth realized that there were inconsistencies in information that families and patients were getting.
J: So we came up with a script for that to walk people through it.
M: That’s the kind of thing we talk about in our UBT meetings. When we started, we met every single week, up until about 6 months ago. Now we meet every other week. For the first two years we met every week for a hour. We always made it an important meeting, we only cancelled one or two meetings in the past 2 1/2 years. We try to say this is important and let’s at least connect. In the last couple months we are trying to keep the meeting to a half an hour -- we’re struggling a bit but it’s in appreciation of other employees’ schedules being disrupted by people being gone for a full hour.
Workflow things -- our clinic is huge, we started some of the efforts on the biggest thing that we all voted on -- something on Jen’s side, where at the end of the night, whoever was the last employee, they were getting stuck with a lot of responsibilities like 20 urine samples sitting, not having orders, and more. That was one of the first things we did.
J: For us on my side where I came from it was big. There was a lot of running around and chasing doctors for orders. So we came out with a strict list of what we do. So at the end of the day someone isn’t left wondering what to do.
M: We tag into the True North metrics and we also continue to do stuff we started last year. The metrics are increasing number of patients. We started with a really low number and we have brought it back to the staff and identified 5 people who wanted to own the process themselves. We asked for volunteers and we were able to make those 5 people “super users” What could they do to support me to support the organization? We did that around MyChart. For telehealth, everyone is doing it, but people were struggling, so we made a little cheat sheet around workflow to make it easier for people.
J: We broke people off into teams and took sections of the doctors -- it was a domino effect, it made everything much easier. It made it a much smoother process after coming back from deployment, in this new transition that nobody really knows well.
M: Jen’s more of the clinical nursing part, but we also have two ASRs who are on our UBT committee. They come to every single meeting and they are helping us with our efforts to collect co-pays. Pre-Covid we were pretty good about collecting copays, but then Covid hit and no one wanted to handle money or credit cards. We fell off and were collecting very little. Many in-persons were telehealth, you can’t make someone pay when they’re at home. So we used their input a lot to brainstorm how we could get better around our co-pays. We made efforts based on what the front desk staff thought and we implemented changes there.
We started this journey about 6 months into the UBT realizing that -- we are attached to the hospital, so not only do we bill for provider visits but we bill for a facility charge. That’s attesting that they use space and rooms and nursing services here. I kept getting a report that we were missing the facility charges. I put a lot of efforts into it initially on my own before the UBT. How can I make sure people see that they didn’t do it? It’s a really busy clinic, these staff were seeing 325 patients a day. They’re busy and they forgot to go back and do it. So I started keeping my eyes on it and we ended up adding a column in our online system so we coil see. Still, things were getting missed. I caught a lot but I was still missing some. So I hired a clinical coordinator with her eyes on it. We were seeing about 50 still missing each month - it was a lot of money. Marie was really excited to know the UBT could be part of a financial gain, so we brought it to UBT. The people at UBT thought, hey, I can own a piece of this, we can have three people also on the floors who are looking at it. So Jen asked who wanted to do it. We were doing better, then COVID hit. And we came back from COVID and a lot of stuff people just forgot what to do. My eyes ended up going back on it. So we started knowing again that a lot is being missed. Recently we just brought it back to UBT, and we came up with a process trying to regain back where we were.
J: When we did it like that, it went from 50 a month then a couple weeks ago it was 0-5 a month. With all of us looking at it.
M: We get like 170$ for that facility fee - it’s graded by level. It’s a lot of money. Two months ago we had zero in the month, first time in ten years. We learned something: of those five, sometimes they were booked as a physical so we did not do them, because we don’t do a facility charge for physicals, or the provider was late or unable to do the physical, or just did a follow-up. But the follow-up DOES need a facility charge -- we didn’t do it because something was scheduled wrong. Working together, we have a really great partnership. Not just with Jen and me, but with everyone on our team. People have been great to go out and share what we are doing with our UBT. Unfortunately, sometimes managers take the brunt of resistance to making change, without the buy-in. But I have my people also speaking to the changes. That's one of the biggest things for me as a manager. Buy-in from the people who are doing it -- people also feel open to saying what isn’t working, or what we need to change.
J: There’s a good open line of communication, it makes it easy to get stuff done and come to people with our problems and concerns, and feel confident that it will at least get addressed. Even if it’s not perfect there will be an effort made.
M: We have a really great UBT team because of the relationships. We’ve been through it from the get-go. We know what works and what doesn’t. We know how we each work. The biggest thing for me as a manager is that I want the change to happen I can try to justify my way, but I am not the solution. So really, the best thing for me is to have this core group of my team communicating workflow issues or changes. It’s great for the team to see that the changes aren’t always easy to roll out, we have to work at it, and sometimes go back to the drawing board.
J: The UBT gives us a better perspective of her responsibilities.
M: They're going to go and work on the details. Just keep it open, they come and say anything to me. IT gets us to where we want to be in the end. Sometimes it’s like, “Holy moly, another thing!” But at the end of the day, our interests are in the staff and the clinic. This is the first time we were a Tier 1 project.
J: An open line of communication is the most important thing for the UBT. The manager being open and receptive to your ideas. Everybody here as the same goal in mind. We work really well together.
M: With that, we have our frustrations. Nothing is perfect here. We just started talking last UBT meeting about trying to understand everyone’s role -- and what people are doing every day. There are some hurt feelings if it seems like someone is working harder than others. So we made a mandatory meeting to discuss and understand better everyone’s roles and how we can all help each other on the team, and how to improve everyone’s workflow. The MNA has joined in our UBT -- we want everyone’s input. Sometimes we are in a meeting and think we have an agenda, but then someone brings up frustration from the floor. We haven’t been getting as many ideas right now, but even to have meetings to have conversations about what is going on in the floor.
J: These are concerns from a week ago and we already have a meeting planned about it.
M: The minutes are always typed up and posted so everyone can read it. There is a good line of communication. After the meetings I always email everyone about the direction we want to move in. The staff can start the conversation -- this is what we are trying to do. You HAVE to get the buy-in, you can't just have one or two people there.
J: It has to be a group effort. The more people that were involved, the easier the solution was to come to.
M: For the wrap up, for me, when you put a dollar amount to it -- the staff all want the organization to be successful. It’s more than just, “you missed something.” Instead it’s, “Oh! We could have gotten an extra 10k this week if we had caught that” I think it led to an instant buy-in. Even from the get-go for us, we had all of those ideas come in, and then in the meeting we typed up all the ideas and asked the staff to pick the top three to work on. That’s how we sorted it. That took 2-3 weeks figuring it out.
J: We kind of went with issues that they already knew were going on. And they saw the issues right in front of their face, that helped.
M: We included everyone in the process. We’d say “we’re doing this because of this, but do you have a better idea?” We’d help teammates figure out the language to explain the changes to the other staff members.
I’m not perfect, I go to the floor and try to help them when they say they’re drowning. I have been in their shoes. I think that is really helpful. I appreciate how hard it is.
J: She doesn’t reprimand. She brings stuff up that gets everyone on board and wants to be proactive about it. You aren’t feeling like you are being singled out or reprimanded. She has a different way of saying hey, we need something else.
M: We are successful because of our partnership amongst ourselves. I’ve told people, well, I remember when I first started UBT, I did feel like “OMG, this is another thing, it’ll be a lot of work” . . . and honestly, it probably was. The first six months to a year, it was a lot — the minutes, communications, updating everyone. Yes, it took effort. But we are in such a better place. The solution isn’t with the manager, it’s with the team. If I didn’t have my team, I’m not successful. I’m only successful because of them -- and having the appreciation that you need buy-in. At the end of the day, it’s them doing most of the work, telling you what is not right out there. I can only assume everything is perfect and then it’s not. If they don’t tell me what isn’t going well, I’m looking pretty foolish if I think I have a wonderfully running clinic. You have to rely on your people. People can join any time they want. We want people to tell us what’s going on, in the meetings or with suggestion notes.
J: Everything was hairy when we came back from deployment. Working with new rules for months and then coming back to a new environment — it was really hard. Even though we are back, it’s completely different.
M: Some people were upset with others. I think when you are away for four months, you do forget some of the stuff. People forgot to do steps in their processes.
We used to have 300+ patients in-house; now it’s 150 in-house and 150 telehealth, so the workflow has still totally changed since Covid.
J: Our workflow is much better now and smoother because everyone knows their roles.
M: We did a video before COVID hit, for the staff. We have done some dancing and singing videos. We have a new one coming out, we are looking to a mask-free summer. We are trying to show the hope we have through our new video that will be coming out. It’ll be out on the UMass page.
J: We do really like each other and we have fun. There has to be a balance. Plus we are with kids, so it’s a different environment. For the patients’ sake, they are coming in scared. When you’re a bit of a goof, it makes them a bit more comfortable.