Marnie Doyle
Virtual Ambassador Program (Pedi Clinic), 5/11/20
Marnie’s family visiting her Mom
Everyone’s got their personal stuff happening right now, so I’m not going to complain about it. I’m very fortunate I was put in this position, and that I’m not sitting home. My manager Maureen told me one Friday you don’t need to come back to clinic next week. I was home a week and got the call. I’m glad it happened. I can’t complain because some people have been deployed to other shifts and tougher assignments. So I feel very grateful and lucky, that’s how I look at it.
As virtual ambassadors, our job is to call into patients’ rooms every day to see how they are doing, whether they need anything, and just connect with them, help them feel less isolated. It’s a new program, and it’s a really great program. I love it actually. I was there for the first day – we trained in groups of six over the course of a day, then got started the next day. We are divided into two rooms in the basement of the ACC building.
We come in in the morning and get an assignment, dividing up the floors between us. We piloted with just a few floors but now we’re calling everybody we can, basically – some patients can’t talk, obviously, and some of these new units don’t have room phones. They have this whole system for us, Cipher, that makes it easy for us to see our notes from the previous day. Most people are really, super appreciative. A few say please don’t bother me again, and that’s ok, you’ll always get those. We ask them if their cell phones are working, how they’re doing connecting with loved ones, whether they need anything, how they’re doing – we just try to have a human conversation really.
I’m enjoying being the patient’s advocate, helping them get what they need. I love that role. They try to set things up such that we can call the same people every day, so we really develop a rapport – certain people even ask for you when someone else calls!
I’d say most conversations are about 5 to 10 minutes long. My longest was with this 94 year-old woman last week, she was teaching me all about World War II, we were on the phone 45 minutes. Those are my favorite conversations – the ones where you can tell the person is just looking for some company. It’s lonely here in the hospital, and I love that I can help people feel less alone, particularly the elderly. Those are the ones that mean the most, because my mother is going through all of this too, and my family is going through it with her.
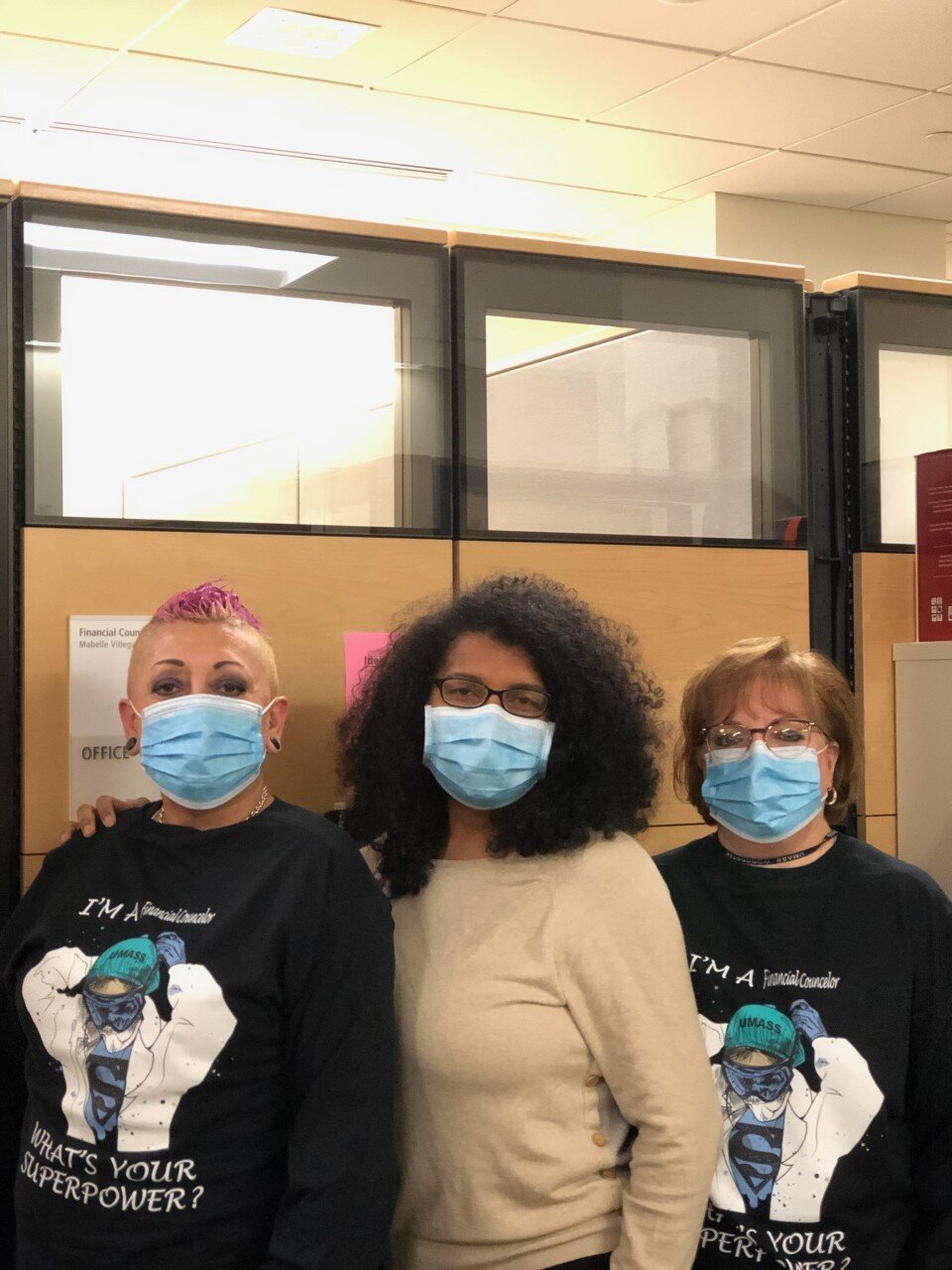
Marnie and her friend Lisa
My Mom was at the Beaumont, so she was affected when they moved everyone out to make it a COVID facility. She has dementia, so that was really hard. She was moved, and it actually turned out fine, but then last week she tested positive. She needs me right now. If someone doesn’t have someone to advocate for them they can get lost in the system. So making sure these patients don’t get lost really matters to me.
There are so many people out there not working so I feel lucky that I can be, and that what I’m doing feels like it matters to people. I know it’s not patient care but at the same time it sort of is, you know? This older guy said to me the other day after we talked “you made my day”, and I just started crying, and then he started crying. I love connecting with people like that. You talk to a lot of people here who are homeless, who have nowhere to go, who have a really tough life outside of here. Helping them feel better, that’s huge. Like I say, the little things are the big things.
We’ve got three SHARE members here, I think, the rest are nurses. We’ve really gelled, and feel proud of the program. One room asks the other whether they need anything so we can all get out of here at the end of the day. I expect I’ll be here a little while, which is okay with me.
Who am I most worried about? I’m most worried about my mom. I’ve got a phone call with the director of the place she’s at this afternoon. You worry about everything. You worry about bringing something home, too, to your family. Everything. Everything.
My best friend of 25 years killed herself last year – this past Tuesday was the one-year anniversary. She was a friend I grew up with and a nurse on 5 East for 20 years. That has been a really hard thing to deal with and go and do my job every day.